Review Guide Reproductive System
In the male reproductive system, the parts and hormones work together to produce. The male animal possesses special reproductive organs. These organs are. Genetics is the science of inheritance, the study of the passage of traits from.
What endocrine glands regulate sexual activity in males? How does this regulation work and what hormones are involved? In males, sexual activity is regulated by the endocrine glands: the hypophysis (the pituitary), the adrenal glands and the gonads (testicles). FSH (follicle-stimulating hormone) secreted by the adenohypophysis acts on the testicles, stimulating spermatogenesis. LH (luteinizing hormone), another adenohypophyseal hormone, also stimulates the production of testosterone by the testicles. Testosterone, the production of which intensifies after the beginning of puberty, acts on several organs of the body and is responsible for the appearance of secondary male sex characteristics (beard, body hair, deep voice, increase in the muscle and bone mass, maturation of genitalia, etc.). Testosterone also stimulates spermatogenesis.
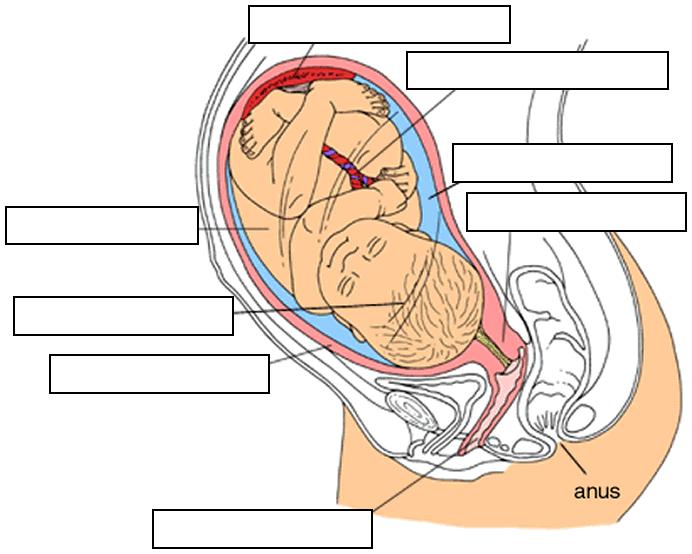
The Reproductive System Review - Image Diversity: The Female Reproductive System. What are the anatomical relationships between the organs of the female reproductive system, from the external vulva to the ovaries? The external female genitalia is called the vulva. The vulva is the external opening of the vaginal canal, or vagina.
The vagina is the copulation organ of females and its posterior extremity communicates with the uterus through the uterine cervix. The uterus is divided into two portions: the cervix and the uterine cavity. The lateral walls of the uterine fundus communicate with the Fallopian tubes. The other extremity of each Fallopian tube ends in fimbria, forming fringes in the abdominal cavity. Between the uterine tube and the ovary is intra-abdominal space. What is the relationship between estrogen level and the LH level in the menstrual cycle?
What is the function of LH in the menstrual cycle and when does its blood concentration reach a peak? The increase in the blood concentration of estrogen with the growing of the ovarian follicle causes the hypophysis to secrete LH.
During this phase, LH acts along with FSH to promote the maturation of the follicle, which on the 14th day, ruptures, releasing the female gamete (ovulation). After the release of the ovum, LH stimulates the formation of the corpus luteum, a structure made from the remaining follicular mass. LH concentration is at its maximum on the 14th day of the cycle. The Reproductive System Review - Image Diversity. Into what structure is the follicle transformed after ovulation?
What is the importance of that structure in the menstrual cycle? The follicle that released the ovum undergoes the action of LH and is transformed into the corpus luteum.
The corpus luteum is very important because it secretes estrogen and progesterone. These hormones prepare the uterine mucosa, also known as endometrium, for nidation (the implantation of the zygote in the uterine wall) and embryonic development, since they stimulate the thickening of the mucous tissue, increase its vascularity and cause the appearance of uterine glycogen-producing glands. How does negative feedback between the hypophysis and corpus luteum work? What is the name given to the atrophied corpus luteum after this feedback process? After ovulation, the estrogen and progesterone secretions from the corpus luteum inhibit hypophyseal FSH and LH secretions (this happens through the inhibition of GnRH, gonadotropin-releasing hormone, a hypothalamic hormone). The blood concentration of these adenohypophyseal hormones falls to basal levels once again.
As LH lowers, the corpus luteum (luteum means “yellow”) becomes atrophic and turns into the corpus albicans (“white”). With the regression of the corpus luteum, the production of estrogen and progesterone ceases. The Reproductive System Review - Image Diversity. Including the main events and hormonal changes, how can the menstrual cycle be described? The cycle can be described like an analog clock on which 12 o’clock is the beginning and the end of the menstrual cycle and 6 o’clock corresponds to the 14th day of the cycle. At 12 o’clock, menses and therefore the menstrual cycle begin and FSH blood levels begins to increase. Around 2 o’clock, the follicles maturing under the effect of FSH are already secreting estrogen and the endometrium is thickening.
Around 3 o’clock, estrogen is intensely stimulating the increase of LH blood levels. At 6 o’clock (the 14th day), LH is at its maximum concentration and FSH is also at high levels to promote ovulation. LH then stimulates the formation of the corpus luteum. Around 7 o’clock, the corpus luteum is already secreting a large amount of estrogen and progesterone and the endometrium thickens even more; levels of FSH and LH decrease with the increasing of the ovarian hormones. Around 11 o’clock, the reduced LH and FSH levels make the corpus luteum turn into the corpus albicans; the production of estrogen and progesterone ceases and the endometrium regresses. At 12 o’clock again (the 28th day), the endometrium desquamates and a new menstrual cycle begins. In general, during what phase of the menstrual cycle can copulation lead to fertilization?
Although this is not a rule, to be effective, fertilization must occur within 24 hours after ovulation (which occurs around the 14th day of the menstrual cycle). Fertilization may occur even if copulation took place up to 3 days before ovulation, since male gametes remain viable for about 72 hours within the female reproductive system. However, the fertile period of the women is considered to be the period from 7 days before ovulation to 7 days after ovulation. How does the sexual arousal mechanism in women facilitate fertilization? During sexual arousal in women, the vagina secretes substances to neutralize its acidity, thus allowing the survival of sperm cells within it. During the female fertile period, hormones make the mucus that covers the internal surface of the uterus less viscous to help the passage of sperm cells into the uterine tubes.
During copulation, the uterine cervix advances inside the vagina to facilitate the entrance of male gametes through the cervical canal. Nidation and Pregnancy. What is tubal pregnancy? Often fertilization takes place in the Fallopian tubes. Generally, the newly formed zygote is moved to the uterus, where nidation and embryonic development occur. However, in some cases, the zygote cannot descend into the uterus and the embryo implants itself in the uterine tube tissue, which is the characteristic of tubal pregnancy. Tubal pregnancy is a severe clinical condition since the tube often ruptures during gestation, causing a hemorrhage and even the death of the woman.
The most common treatment for tubal pregnancy is surgery. Does the hypophysis-ovaries endocrine axis work in the same way during pregnancy as in non-pregnant women? If pregnancy does not occur how does another menstrual cycle begin? The functioning of the hypophysis is altered during pregnancy. Since estrogen and progesterone levels remain elevated during the gestational period, the production of GnRH (gonadotropin-releasing hormone) from the hypothalamus is inhibited. The lack of GnRH therefore inhibits the secretion of FSH and LH by the hypophysis and a new menstrual cycle does not begin.
If pregnancy does not occur, the lowering of estrogen and progesterone levels stimulates the production of GnRH by the hypothalamus. This hormone then hastens the adenohypophyseal secretion of FHS and LH, which in turn stimulate the maturation of follicles and the beginning of a new menstrual cycle. What is the endocrine function of the placenta? The placenta, in addition to being the organ through which the exchange of substances between the mother and the fetus is carried out, also has the function of secreting estrogen and progesterone to maintain a high level of these hormones during pregnancy.
(The placenta still secretes other hormones such as human placental lactogen, which acts in a way similar to that of the hypophyseal hormones that regulate reproduction, and HCG, human chorionic gonadotropin.) Reproductive Planning Methods. What are the common contraindications of contraceptive pills? There are medical reports associating the use of contraceptive pills with vomiting, nausea, vertigo, headaches, hypertension and other pathological conditions. Some research has attempted to relate the medical ingestion of estrogen and progesterone with an increased propensity for cardiovascular diseases (such as heart attacks, strokes and thrombosis) and malignant neoplasms (cancers). Doctors must always be asked about the risks and benefits of the contraceptive pill prior to use. What are the most common methods of male and female surgical sterilization? Vasectomy is the most common method of surgical sterilization in men.
In vasectomy, the vas deferens inside the scrotum are sectioned and closed at a section, forbidding the sperm cells from entering the ejaculatory duct but still allowing the release of seminal fluid during ejaculation. The surgical sterilization of women is often done by bilateral tubal ligation. With tubal ligation, the ovum does not enter the uterus and, as a result, sperm cells cannot reach it. The Reproductive System Review - Image Diversity. What is the normal duration of the menstrual cycle?
How does the calendar contraceptive method work? The normal duration of the menstrual cycle is 28 days, but it can vary among different women or different cycles in the same woman.
In the calendar contraceptive method, the date n-14 (n minus 14) is taken, considering n the number of days of the normal menstrual cycle of the woman (generally n=28). The safety margin +3 or –3 refers to the days around n-14 during which intercourse should be avoided to prevent pregnancy. (This method is not completely free of failures. A doctor must always be consulted before relying on any contraceptive method.).
What is the contraceptive mechanism of an IUD? An IUD (intrauterine device) is a piece of plastic coated with copper that is inserted into the uterus by a doctor. Copper is then gradually released (an IUD can last from 5 to 10 years) and since it has a spermicidal effect, sperm cells are destroyed before fertilization. In addition to this mechanism, the movement of the IUD inside the uterus causes slight endometrial inflammation, which helps to prevent nidation.
The Reproductive System Review - Image Diversity: Reproduction in Other Animals (See zoology subjects for a comprehensive review.). Generally, how does a male animal realize that the female is receptive to copulation? In most vertebrate species with internal fertilization, females have reproductive cycles with fertile periods. During this period, the female secretes pheromones (odoriferous substances that attract the male of the species) from the skin and mucosae. The presence of the male individual and his pheromones also stimulates the release of pheromones by the female. (Many animals also use pheromones to mark their territories and for signal transmission between individuals about the location of dangers and food.). What is parthenogenesis?
Parthenogenesis is the reproduction or formation of a new individual from the egg cell without fertilization by the male gamete. Depending on the species, individuals born via parthenogenesis may be male or female, or of any sex. In bees, the drone (the single male bee) is haploid and born via parthenogenesis while the females (queen and workers) are diploid. Now that you have finished studying, these are your options:.
Review this subject, read all Q&As again. Study the next subject: go to. Choose another Q&A sequence to study by using the subject menu.
. The ovary is the organ that produces ova (singular, ovum), or eggs. The two ovaries present in each female are held in place by the following ligaments:. The broad ligament is a section of the peritoneum that drapes over the ovaries, uterus, ovarian ligament, and suspensory ligament. It includes both the mesovarium and mesometrium.
The mesovarium is a fold of peritoneum that holds the ovary in place. The suspensory ligament anchors the upper region of the ovary to the pelvic wall. Attached to this ligament are blood vessels and nerves, which enter the ovary at the hilus. The ovarian ligament anchors the lower end of the ovary to the uterus. The following two tissues cover the outside of the ovary:.
The germinal epithelium is an outer layer of simple epithelium. The tunica albuginea is a fibrous layer inside the germinal epithelium. =The inside of the ovary, or stroma, is divided into two indistinct regions, the outer cortex and the inner medulla. Embedded in the cortex are saclike bodies called ovarian follicles. Each ovarian follicle consists of an immature oocyte (egg) surrounded by one or more layers of cells that nourish the oocyte as it matures. The surrounding cells are called follicular cells, if they make up a single layer, or granulosa cells, if more than one layer is present.
The uterine tubes (oviducts) transport the secondary oocytes away from the ovary and toward the uterus (the ovaries consist of primary oocytes, which develop into secondary oocytes). The following regions characterize each of the two uterine tubes (one for each ovary). The infundibulum is a funnel‐shaped region of the uterine tube that bears fingerlike projections called fimbriae.
Pulsating cilia on the fimbriae draw the secondary oocyte into the uterine tube. The ampulla is the widest and longest region of the uterine tube. Fertilization of the oocyte by a sperm usually occurs here. The isthmus is a narrow region of the uterine tube whose terminus enters the uterus. The wall of the uterine tube consists of the following three layers:. The serosa, a serous membrane, lines the outside of the uterine tube. The middle muscularis consists of two layers of smooth muscle that generate peristaltic contractions that help propel the oocyte forward.
The inner mucosa consists of ciliated columnar epithelial cells that help propel the oocyte forward, and secretory cells that lubricate the tube and nourish the oocyte. The uterus (womb) is a hollow organ within which fetal development occurs. The uterus is characterized by the following regions:. The fundus is the upper region where the uterine ducts join the uterus. The body is the major, central portion of the uterus.
The isthmus is the lower, narrow portion of the uterus. The cervix is a narrow region at the bottom of the uterus that leads to the vagina. The inside of the cervix, or cervical canal, opens to the uterus above through the internal os and to the vagina below through the external os.
Cervical mucus secreted by the mucosa layer of the cervical canal serves to protect against bacteria entering the uterus from the vagina. If an oocyte is available for fertilization, the mucus becomes thin and slightly alkaline.
These are attributes that promote the passage of sperm. At other times, the mucus is viscous and impedes the passage of sperm. The uterus is held in place by the following ligaments:. Broad ligaments. Uterosacral ligaments. Round ligaments.
Cardinal (lateral cervical) ligaments The wall of the uterus consists of the following three layers:. The perimetrium is a serous membrane that lines the outside of the uterus. The myometrium consists of several layers of smooth muscle and imparts the bulk of the uterine wall. Contractions of these muscles during childbirth help force the fetus out of the uterus. The endometrium is the highly vascularized mucosa that lines the inside of the uterus. If an oocyte has been fertilized by a sperm, the zygote (the fertilized egg) implants on this tissue.
The endometrium itself consists of two layers. The stratum functionalis (functional layer) is the innermost layer (facing the uterine lumen) and is shed during menstruation. The outermost stratum basalis (basal layer) is permanent and generates each new stratum functionalis. The vagina (birth canal) serves both as the passageway for a newborn infant and as a depository for semen during sexual intercourse. The upper region of the vagina surrounds the protruding cervix, creating a recess called the fornix.
The lower region of the vagina opens to the outside at the vaginal orifice. A thin membrane called the hymen may cover the orifice.
The vaginal wall consists of the following layers:. The outer adventitia holds the vagina in position.
The middle muscularis consists of two layers of smooth muscle that permit expansion of the vagina during childbirth and when the penis is inserted. The inner mucosa has no glands.
But bacterial action on glycogen stored in these cells produces an acid solution that lubricates the vagina and protects it against microbial infection. The acidic environment is also inhospitable to sperm.
The mucosa bears transverse ridges called rugae. The vulvae (pudendum) make up the external genitalia. The following structures are included:. The mons pubis is a region of adipose tissue above the vagina that is covered with hair. The labia majora are two folds of adipose tissue that border each side of the vagina. Hair and sebaceous and sudoriferous glands are present.
Developmentally, the labia majora are analogous to the male scrotum. The labia minora are smaller folds of skin that lie inside the labia majora.
The vestibule is the recess formed by the labia minora. It encloses the vaginal orifice, the urethral opening, and ducts from the greater vestibular glands whose mucus secretions lubricate the vestibule.
The clitoris is a small mass of erectile and nervous tissue located above the vestibule. Extensions of the labia minora join to form the prepuce of the clitoris, a fold of skin covering the clitoris. Figure 1. View of the female reproductive system. Mammary glands The mammary glands are sudoriferous (sweat) glands specialized for the production of milk. The milk‐producing secretory cells form walls of bulb‐shaped chambers called alveoli that join together with ducts, in grapelike fashion, to form clusters called lobules.
Numerous lobules assemble to form a lobe. Each breast contains a single mammary gland consisting of 15 to 20 of these lobes. Lactiferous ducts leading away from the lobes widen into lactiferous sinuses that serve as temporary reservoirs for milk. The ducts narrow again as they lead through a protruding nipple. The nipple, whose texture is made coarse by the presence of sebaceous glands, is surrounded by a ring of pigmented skin called the areola.
Contraction of myoepithelial cells surrounding the alveoli force milk toward the nipples. The breasts begin to enlarge in females at the onset of puberty. Proliferating adipose (fat) tissue expands the breast, while suspensory ligaments attached to the underlying fascia provide support. In nonpregnant females (and in males), the glands and ducts are not fully developed. During pregnancy, estrogen and progesterone stimulate extensive development of the mammary glands and associated ducts. After childbirth, various hormones, especially prolactin from the anterior pituitary, initiate lactation, or milk production. When neurons are stimulated by the sucking of an infant, nerve impulses activate the posterior pituitary to secrete oxytocin, which in turn stimulates contraction of the myoepithelial cells surrounding the alveoli.
Milk is then forced toward the nipple (the letdown reflex). Oogenesis Oogenesis consists of the meiotic cell divisions that lead to the production of ova (eggs) in females.
The process begins during fetal development with the fetal ovary. Diploid cells called oogonia divide by mitosis and differentiate to produce primary oocytes (still diploid with 46 chromosomes). Each primary oocyte is encircled by one or more layers of cells. The oocyte and encircling cells together are called an ovarian follicle.
The primary oocytes (within their follicles) begin meiosis, but division progresses only to prophase I. They remain at this stage until puberty. The following stages in the development of an ovarian follicle are observed:. The primordial follicle, the initial fetal state of the follicle, encircles the oocyte with a single layer of cells, called follicular cells. The primary follicle, the next stage of follicular development, possesses two or more layers of encircling cells, now called granulosa cells.
The secondary follicle is distinguished by the presence of the antrum, a fluid‐filled, central cavity. In a mature (vesicular, or Graafian) follicle, the primary oocyte has completed meiosis I. It is the stage of follicular development that precedes ejection of the oocyte from the ovary (ovulation).
The following features are observed:. The zona pellucida, a clear layer of glycoprotein, surrounds the oocyte.
The corona radiata, a ring of granulosa cells, encircles the zona pellucida. Several layers of cells (theca cells) surround the granulosa cells. The corpus luteum is the remains of the follicle following ovulation. It remains functional, producing estrogen, progesterone, and inhibin, until it finally degenerates.
During each menstrual cycle, one primary oocyte, enclosed in its follicle, resumes meiosis I to produce two daughter cells (each haploid with 23 chromosomes). One daughter cell, the secondary oocyte, contains most of the cytoplasm, ensuring that adequate amounts of stored food, as well as mitochondria, ribosomes, and other cytoplasmic organelles, will be available for the developing embryo. The other daughter cell, a first polar body, is much smaller and contains little cytoplasm and few if any organelles.
Functions Of The Reproductive System
The secondary oocyte then begins meiosis II (equatorial division) but again stops at prophase (this time prophase II). The first polar body may also begin meiosis II, but it will eventually degenerate. Ovulation occurs when a secondary oocyte and its first polar body, surrounded by the zona pellucida and corona radiata, rupture from their mature follicle and are expelled from the surface of the ovary.
The oocyte is then swept up into the uterine (fallopian) tube and advances toward the uterus. If a sperm cell penetrates the corona radiata and zona pellucida and enters the secondary oocytes, meiosis II resumes in the secondary oocytes, producing an ovum and a second polar body. If a first polar body is present, it too, may resume meiosis II, producing daughter polar bodies. Fertilization occurs when the nuclei of the sperm cell and ovum unite, forming a zygote (fertilized egg). Any polar bodies present ultimately degenerate. Hormonal regulation of oogenesis and the menstrual cycle The human female reproductive cycle is characterized by events in the ovary (ovarian cycle) and the uterus (menstrual cycle). The purpose of these cycles is to produce an egg and to prepare the uterus for the implantation of the egg, should it become fertilized.
The ovarian cycle consists of three phases:. The follicular phase describes the development of the follicle, the meiotic stages of division leading to the formation of the secondary oocytes, and the secretion of estrogen from the follicle. Ovulation, occurring at midcycle, is the ejection of the egg from the ovary.
The luteal phase describes the secretion of estrogen and progesterone from the corps luteum (previously the follicle) after ovulation. The menstrual (uterine) cycle consists of three phases:. The proliferative phase describes the thickening of the endometrium of the uterus, replacing tissues that were lost during the previous menstrual cycle. The secretory phase follows ovulation and describes further thickening and vascularization of the endometrium in preparation for the implantation of a fertilized egg.
The menstrual phase (menstruation, menses) describes the shedding of the endometrium when implantation does not occur. The activities of the ovary and the uterus are coordinated by negative‐ and positive‐feedback responses involving gonadotropin releasing hormone (GnRH) from the hypothalamus, follicle stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary, and the hormones estrogen and progesterone from the follicle and corpus luteum. A description of the events follows):.
The hypothalamus and anterior pituitary initiate the reproductive cycle: The hypothalamus monitors the levels of estrogen and progesterone in the blood. In a negative‐feedback fashion, low levels of these hormones stimulate the hypothalamus to secrete GnRH, which in turn stimulates the anterior pituitary to secrete FSH and LH. The follicle develops: FSH stimulates the development of the follicle from primary through mature stages. The follicle secretes estrogen: LH stimulates the cells of the theca interna and the granulosa cells of the follicle to secrete estrogen. Inhibin is also secreted by the granulosa cells. Ovulation occurs: Positive feedback from rising levels of estrogen stimulate the anterior pituitary (through GnRH from the hypothalamus) to produce a sudden midcycle surge of LH. This high level of LH stimulates meiosis in the primary oocyte to progress toward prophase II and triggers ovulation.
The corpus luteum secretes estrogen and progesterone: After ovulation, the follicle, now transformed into the corpus luteum, continues to develop under the influence of LH and secretes both estrogen and progesterone. The endometrium thickens: Estrogen and progesterone stimulate the development of the endometrium, the inside lining of the uterus. It thickens with nutrient‐rich tissue and blood vessels in preparation for the implantation of a fertilized egg. The hypothalamus and anterior pituitary terminate the reproductive cycle: Negative feedback from the high levels of estrogen and progesterone cause the anterior pituitary (through the hypothalamus) to abate the production of FSH and LH. Inhibin also suppresses production of FSH and LH. The endometrium either disintegrates or is maintained, depending on whether implantation of the fertilized egg occurs, as follows:. Implantation does not occur: In the absence of FSH and LH, the corpus luteum deteriorates.
As a result, estrogen and progesterone production stops. Without estrogen and progesterone, growth of the endometrium is no longer supported, and it disintegrates, sloughing off during menstruation.
Implantation occurs: The implanted embryo secretes human chorionic gonadotropin (hCG) to sustain the corpus luteum. The corpus luteum continues to produce estrogen and progesterone, maintaining the endometrium. (Pregnancy tests check for the presence of hCG in the urine.) In addition to influencing the reproductive cycle, estrogen stimulates the development of secondary sex characteristics in females.
Reproductive System Powerpoint Presentation
These include the distribution of adipose tissue (to the breasts, hips, and mons pubis), bone development leading to a broadening of the pelvis, changes in voice quality, and growth of various body hair. Figure 2. The female reproductive cycle broken down by days.
Comments are closed.